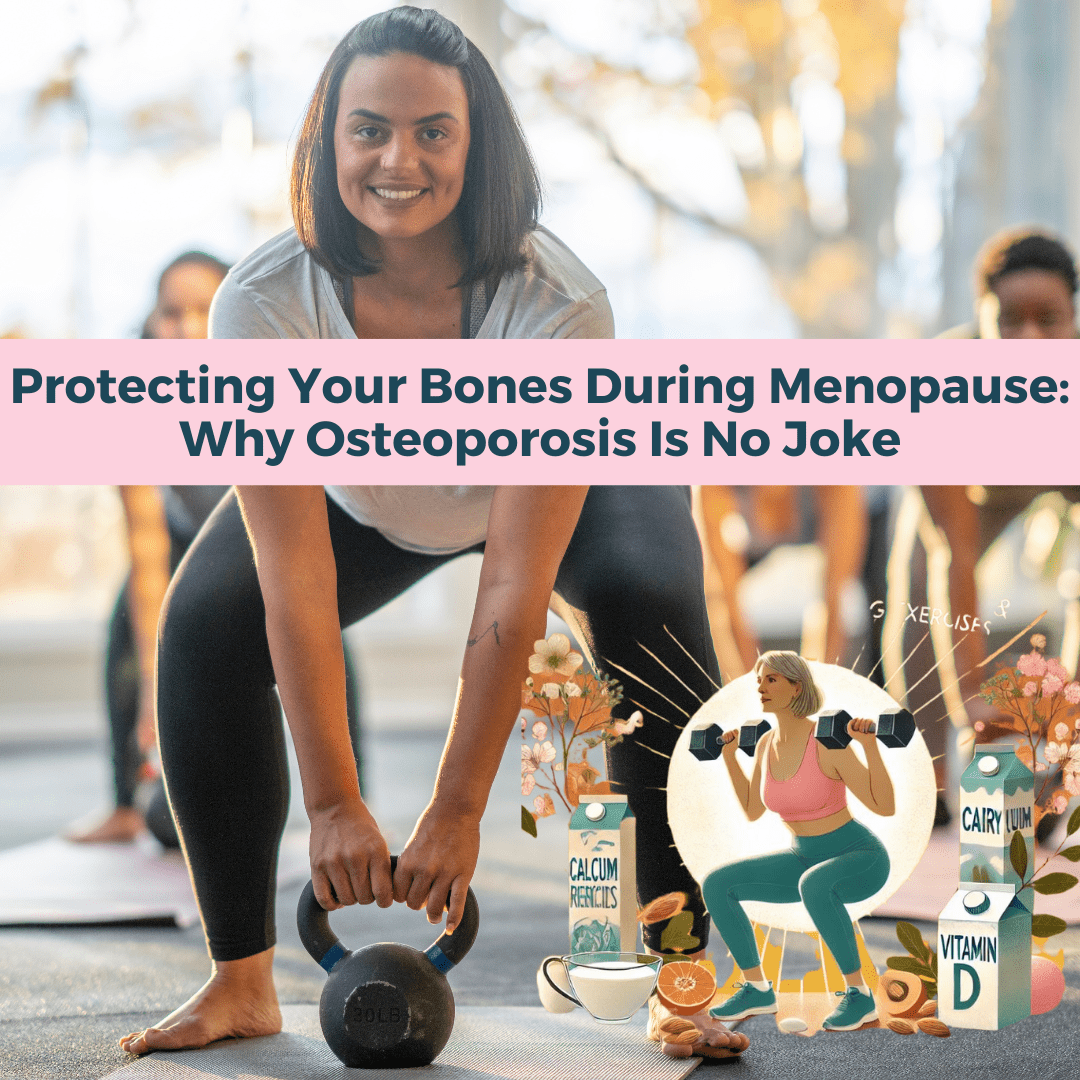
Protecting Your Bones During Menopause: Why Osteoporosis Is No Joke
Protecting Your Bones During Menopause: Why Osteoporosis Is No Joke Osteoporosis is no joke—it's the most common bone disorder in the world and affects far more people than you might think. In fact, around half of women over 50 will break a bone due to osteoporosis, and men aren’t immune either, with 20% facing the same risk. This condition is especially dangerous when it leads to hip fractures, which come with serious consequences, including disability and even death. A staggering 21% of people who have hip fractures surgically repaired do not survive past a year, and that number jumps to 70% if the fracture isn’t repaired. With the aging population, experts estimate that the number of people with osteoporosis will double in the next 20 years. This is a huge wake-up call for women, particularly those entering menopause—a time when bone health really starts to take a hit. Let’s dive into what you need to know about protecting your bones during this critical stage of life! The Menopause-Osteoporosis Connection: Why It Matters Menopause is a game-changer, especially when it comes to bone health. Osteoporosis and associated fractures are the most common metabolic bone diseases and represent a major global health problem, contributing to 8.9 million fractures worldwide each year. Most women don’t realize that their risk of osteoporosis skyrockets as they enter menopause, and this isn’t just about “getting older.” It’s about our hormones—specifically, the loss of estrogen, progesterone, and testosterone, which play vital roles in maintaining bone density.
Key Factors Impacting Bone Density
Several key factors can impact bone density in women, especially as we age:
- Age: Bone density naturally declines as we get older, particularly after menopause when hormone levels plummet. Women who experience early menopause or have had their ovaries removed are at an even higher risk for osteoporosis due to this hormonal shift.
- Genetics: If osteoporosis runs in your family, you may be more likely to develop it yourself.
- Nutrition: Ensuring you get enough calcium and vitamin D is crucial for bone health; a deficiency in these nutrients can increase your risk of osteoporosis.
- Lifestyle Factors: Sedentary habits, smoking, excessive alcohol consumption, and low body weight can all weaken your bones over time.
- Medical Conditions: Conditions such as celiac disease, hyperthyroidism, and certain autoimmune disorders can negatively impact bone density.
Taking Action for Bone Health The good news? There’s plenty you can do to protect your bones. Regular weight-bearing exercise, HRT, a nutrient-rich diet, avoiding smoking and excessive alcohol, and managing any medical conditions affecting your bone health are all smart strategies. It’s never too early—or too late—to take action!
How Your Hormones Impact Bone Health
- Regulating Bone Remodeling Estradiol and testosterone play key roles in balancing bone resorption (breakdown) and bone formation. Estradiol reduces osteoclast activity (the cells that break down bone), while testosterone stimulates osteoblasts (the cells that build new bone). This balance helps maintain bone density and strength.
- Promoting New Bone Growth Progesterone and testosterone are vital for stimulating osteoblasts to build new bone tissue, ensuring that bones are continually renewed and kept strong, especially as women age.
- Preventing Bone Loss in Menopause All three hormones—estradiol, progesterone, and testosterone—help mitigate the rapid bone loss that occurs during menopause. Estradiol’s protective role against bone breakdown, combined with progesterone and testosterone’s bone-building effects, slows the progression of osteoporosis and reduces fracture risk.
- Supporting Muscle Mass Testosterone supports muscle strength, which helps protect bones by improving balance and reducing the risk of falls—one of the leading causes of fractures in older women.
- Participants Over 1,000 postmenopausal women aged 50–65 receiving either estradiol HRT or a placebo.
- Duration Followed for up to 5 years, with regular measurements of bone mineral density (BMD) in high-risk areas like the hips and spine.
- Method Bone density was measured using dual-energy X-ray absorptiometry (DEXA), the gold standard for assessing bone health.
- Significant Increase in BMD Women on estradiol HRT showed a significant increase in BMD, especially in the lumbar spine and hip, the areas most susceptible to osteoporotic fractures.
- Reduction in Fracture Risk Women receiving estradiol HRT had a 30-50% reduction in the risk of osteoporotic fractures, with the most pronounced benefits seen in those who started therapy closer to menopause.
- Bone Loss Prevention Estradiol plays a crucial role in preventing the rapid bone loss typical during the postmenopausal period. Women on estradiol therapy maintained higher bone density than those not on HRT.
- Increased BMD Women taking bioidentical progesterone alongside estradiol experienced a significantly greater increase in BMD compared to those on estradiol-only therapy.
- Osteoblast Activation Bioidentical progesterone appeared to stimulate osteoblast activity, contributing to increased bone density.
- Reduced Fracture Risk The group receiving bioidentical progesterone had a 30% lower risk of osteoporotic fractures compared to the estradiol-only group.
- Safety and Tolerability Bioidentical progesterone was well-tolerated, with no significant adverse effects.
Nutrients for Bone Protection
Calcium, vitamin D, and magnesium are crucial for maintaining bone health, especially in older adults. Here’s how each nutrient contributes to bone integrity:Calcium
- Bone Structure and Density Calcium is a fundamental component of bone tissue, providing structural support and strength. A deficiency can lead to decreased bone density, increasing the risk of fractures and osteoporosis.
- Recommended Intake Older adults should aim for about 1,200 mg of calcium daily to help mitigate age-related bone loss.
Vitamin D
- Calcium Absorption Vitamin D is essential for absorbing calcium in the intestines. Without adequate vitamin D, the body struggles to utilize calcium, weakening bones.
- Bone Remodeling It also aids in bone remodeling, helping to maintain healthy bone density. Older adults often have lower vitamin D levels due to decreased skin synthesis and dietary intake, negatively impacting bone health.
- Recommended Intake The recommended dietary allowance (RDA) for vitamin D is about 800 to 1,000 IU daily for older adults.
Magnesium
- Bone Formation Magnesium supports bone structure and plays a role in converting vitamin D to its active form, enhancing calcium absorption.
- Preventing Osteoporosis Adequate magnesium intake may help prevent osteoporosis by influencing bone density and turnover. Low magnesium levels are associated with a higher risk of fractures in older adults.
- Recommended Intake The RDA for magnesium is approximately 320 mg per day for women and 420 mg for men.
How Weightlifting Impacts Bone Health
Weightlifting has a significant positive impact on bone health, especially in older adults. Here’s a detailed overview of its benefits:- Bone Density Improvement Weightlifting applies mechanical stress to bones, stimulating formation and increasing density. This is particularly vital for postmenopausal women and older adults at higher risk for osteoporosis and fractures.
- Muscle-Bone Connection Strong muscles support bones, reducing fall risk and fractures. Resistance training builds muscle strength while enhancing balance and coordination.
- Hormonal Response Weightlifting boosts the production of hormones like testosterone and growth hormone, which support bone density and overall health.
- Increased Strength and Flexibility Regular strength training enhances physical function, making daily activities easier and reducing injury risk.
Statistics on Weightlifting and Bone Health
- Bone Density Increases Resistance training can lead to a 1-3% increase in bone mineral density annually, a significant improvement considering age-related declines.
- Fracture Risk Reduction A meta-analysis found that resistance training can reduce fracture risk by 30-50% in older adults.
- Exercise Guidelines The American College of Sports Medicine recommends muscle-strengthening activities on 2 or more days per week as part of a balanced exercise program to improve bone health.
- Postmenopausal Women Weight training has been shown to reduce bone loss in critical areas like the lumbar spine and hip, where fracture risk is high.
Sources:
National Institutes of Health: Osteoporosis and Exercise American College of Sports Medicine: Exercise and Bone Health Journal of Bone and Mineral Research NIH: Calcium and Bone Health NIH: Vitamin D and Bone Health NIH: Magnesium and Bone Health https://link.springer.com/article/10.1007/BF00316876 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4286655/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2968416/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3098904/
Find Karen Martel on Apply Podcast
Karen Martel is a Certified Hormone Specialist and Transformational Nutrition Coach dedicated to empowering women through their health journeys.
As the host of the popular podcast The Hormone Solution, Karen tackles the complexities of hormonal health, weight loss resistance, and the challenges that come with perimenopause and menopause.
Her mission is to disrupt outdated narratives surrounding women's health, providing reliable information and practical solutions that help women reclaim their vitality. With personal experience overcoming her own health struggles, Karen offers insights into hormone optimization and sustainable weight management strategies.
Join her as she engages in enlightening conversations with experts and shares actionable advice, all aimed at helping women navigate their unique hormonal landscapes with confidence and clarity. Tune in to discover how to embrace life's stages while enhancing overall well-being.